Asymmetrical inflamed joints
Hope for those suffering from peripheral spondyloarthritis
By Els Verweire
This article originally appeared in Dutch in EOS Magazine. Read more at eoswetenschap.eu.
Patients with peripheral spondyloarthritis face a lifetime of medication, as this rheumatic condition rarely or never spontaneously disappears. Researchers from the VIB-UGent Center for Inflammation Research and UZ Gent are exploring alternative approaches.
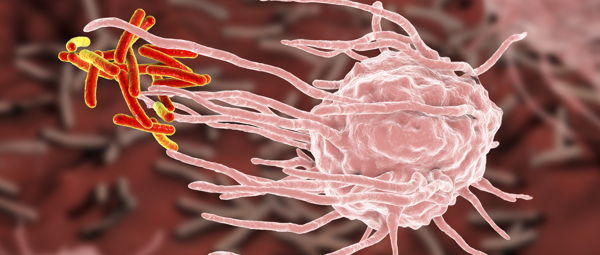
Chronically inflamed and swollen joints make movement painful and difficult. It sounds like something that only affects the elderly. However, in one percent of the population, the first symptoms emerge between the ages of fifteen and thirty-five. They suffer from peripheral spondyloarthritis, a rheumatic condition that targets the joints and tendons of the lower limbs in an asymmetrical manner (see sidebar).
Similar to many other forms of rheumatism, the exact cause of the condition is not entirely clear. The only certainty is a programming error in the immune system. This causes immune cells to not only target harmful organisms that can cause serious infections but also attack harmless structures within the body. This deviation is likely due to a combination of genetic predisposition and environmental factors, such as mechanical joint overloading, bacterial infection by specific microorganisms, or an abnormal composition of the gut flora.

Lifelong medication
To combat symptoms, most patients are prescribed NSAIDs (non-steroidal anti-inflammatory drugs), traditional anti-inflammatory drugs such as diclofenac, piroxicam, or ibuprofen. While these provide pain relief, they inadequately suppress the inflammatory process in their joints and tendons. Therefore, additional disease-modifying treatments, such as sulfasalazine and methotrexate, also known as DMARDs (Disease Modifying AntiRheumatic Drugs), are often necessary.
However, these drugs also have drawbacks. "It often takes several months before the patient feels an effect," says Prof. Dr. Filip Van den Bosch, a rheumatologist at UZ Gent. "And the therapy can cause burdensome side effects, such as nausea and liver and blood disorders."
If DMARDs fail to suppress the inflammatory process and alleviate pain, a step-up therapy with stronger medications like TNF blockers (etanercept, adalimumab, infliximab, certolizumab, golimumab, etc.) is recommended. These are newer and more expensive biological drugs based on substances naturally present in the human body. They block the action of tumor necrosis factor TNF, an inflammatory molecule crucial in joint inflammation. They restore the disturbed function of the immune system and block the inflammation signals it wrongly triggers.
But they too have side effects, including local reactions of the skin at the injection site, allergy and psoriasis flare-ups, headache, dizziness, and an increased susceptibility to infections. The disease rarely or never disappears spontaneously. As a result, patients diagnosed with peripheral spondyloarthritis today are reliant on treatment for a lifetime, whether they continue with standard treatment or switch to biological agents over time.
Promising result
Several years ago, researchers from the VIB-UGent Center for Inflammation Research and UZ Gent wanted to explore a different approach. They aimed to determine if they could make patients symptom-free in the long term by treating them intensively with only biological drugs in the early stages of the disease. The goal was to prevent patients from needing permanent medication.
In 2017, they initiated the clinical study CRESPA (Clinical REmission in peripheral SPondyloArthritis) and identified sixty patients with symptoms detected no longer than twelve weeks prior. "It was no easy task," says Prof. Dr. Dirk Elewaut (VIB, UZ Gent, UGent), head of rheumatology at UZ Gent and a collaborator on the study. "One of the challenges in this search was that painful, swollen joints can have many causes, leading to a significant delay before patients receive a correct diagnosis. In the patients we follow in the Be-GIANT registry (Belgian Inflammatory Arthritis and Spondylitis Cohort, see sidebar), this diagnostic delay averaged 2.4 years. In the United States, it can extend up to ten to fourteen years for certain forms of spondyloarthritis."
Once the researchers gathered the sixty patients, they administered a placebo to a third of them and a TNF blocker to the rest. "The purpose of the placebo group was to definitively prove that patients with peripheral spondyloarthritis rarely spontaneously recover," explains Elewaut. "And we were able to prove that effectively. After 24 weeks, 75 percent of the patients in the anti-TNF group were completely symptom-free, compared to twenty percent in the placebo group."
The scientists further focused their research on the patients who were symptom-free for six months due to treatment. They discontinued the treatment entirely to check if the condition was permanently eliminated. Half of the subjects showed no relapse long after the study concluded.

Follow-up research
The researchers were ecstatic about this promising result and immediately planned the Spartacus project, a more extensive follow-up study with a larger group of subjects to delve deeper into the findings of the small-scale CRESPA study. They are currently in the process of recruiting 120 patients, with half receiving standard treatment, possibly with biological agents as a step-up therapy, and the other half immediately receiving biological agents. This distribution is randomized and double-blind, ensuring neither the scientists nor the subjects know which group they are in during the experiment.
One of the aspects the researchers want to demonstrate in the Spartacus project is the superiority of intensive therapy over standard treatment. "In the CRESPA study, we showed that biological agents work better than a placebo," says Elewaut, the principal investigator of the Spartacus project. "Now we want to investigate if they also work better than standard therapy."
Additionally, the researchers want to determine if the duration of symptoms had an impact on the treatment's effectiveness. "We will make a distinction between patients with symptoms for less than three months and others who had problems for more than three months but less than a year," says Elewaut. "This way, we aim to find out the optimal timing and disease stage to initiate treatment."
Different profiles
Assuming the researchers can replicate the results of the CRESPA study and successfully discontinue therapy in half of the patients, the Spartacus project aims to understand why this works for some patients and not for others. For this purpose, at the beginning of the study, they take a biopsy of the synovial tissue (a thin layer of synovial membrane that produces joint fluid) from the affected joints of each subject and apply the latest techniques.
"With single-cell RNA sequencing, we can analyze all RNA molecules in each individual cell," explains Elewaut. "This allows us to determine which genes are activated or deactivated in each cell and understand how the expression profile of all those cells – from connective tissue cells to immune cells – differs in patients who respond to the therapy and those who do not."
"We hope to find measurable indicators, biomarkers, that can predict which patients will benefit from the innovative treatment strategy and which won’t – something that is not currently possible. And, of course, why that is the case." - Prof. Dirk Elewaut
Additionally, throughout the study, the researchers also plan to collect blood samples from all patients regularly. The goal is to understand why patients who recently developed the disease still respond to treatment while those who have had symptoms for a long time no longer do. “For all rheumatic diseases, if they persist for a while, they become more challenging to treat," explains Elewaut. "One hypothesis is that inflammation induces changes in the epigenetic profile, the layer atop the DNA of each cell that permanently activates or deactivates certain genes. This may reach a point where treatment is no longer effective. We want to investigate this further."
Perspective
The team aims to complete the clinical study by the end of 2024.
"We are still actively working, and we don't have results yet, but we hope to demonstrate that the new therapy works better than standard treatment and that we can also identify who will benefit from the treatment and why," says Elewaut. "If successful, we can offer young people who would otherwise need lifelong medication the prospect of a temporary treatment that can permanently relieve them of their symptoms. This would provide us with scientific evidence to convince the government to consider reimbursing this strategy."
"If successful, we can offer young people who would otherwise need lifelong medication the prospect of a temporary treatment that can permanently relieve them of their symptoms." - Prof. Dirk Elewaut
Due to the potential reimbursement, the researchers appointed a health economist to assess whether the benefits of the new strategy for patients outweigh the costs for society. "I am convinced that if we can prove that we can make half of the patients symptom-free without the need for permanent medication, the treatment will be a health economic asset over standard treatment," says Elewaut. "Even though the new treatment is initially more expensive and needs to be paired with a test to determine who will respond to the treatment, patients will be free from medication for the rest of their lives after six months, significantly reducing costs for society."
Want to be kept up-to-date on our biotechnological news and stories? Join our community and subscribe to our bi-monthly newsletter.
Read more