Dendritic cell atlas: roadmap to a better anti-cancer therapy
-written by Aarushi Audhut Caro, a PhD student at the VIB Center for Inflammation Research
One out of two patients with advanced-stage ovarian cancer dies within five years after diagnosis. Ovarian cancer is often called a silent killer because the symptoms associated with it are very vague and common, including bloating, loss of appetite, belly pain, and frequent urination. As a result, 80% of the patients initially either disregard these symptoms or are misdiagnosed. By the time the correct diagnosis of ovarian cancer is made, the patients are often in the late stages in which the cancer has already spread to other parts of the body. In many cases, this is too late! Interestingly, the majority of late-stage patients occasionally respond positively to the therapies they are provided with, and it appears that the cancer is gone. But eventually, the cancer comes back. Only this time, it’s much more aggressive and does not respond to therapies any longer. Ultimately, it is the late diagnosis and therapy resistance that eventually leads to low five-year survival in ovarian cancer patients. So, it is obvious that we need new therapies that are not only effective but have long-term effects so that late-stage ovarian cancer patients can live more than five years.
Fortunately, our bodies have an elaborate built-in defense system called the immune system, which has great potential to fight not just ovarian but any cancer. Particularly, the dendritic cells of the immune system, work as the security guards of our body. Their job is to constantly patrol every corner of the body for issues, such as infections or tumors. Once they detect an issue, such as a tumor, they immediately instruct the killer cells of the immune system to destroy it.

Interestingly, some dendritic cells can be found living inside the tumor. My research group (Lab of Dendritic Cell Biology and Cancer Immunotherapy at the VIB Center for Inflammation Research) actively investigates the use of these tumor dendritic cells as an anti-cancer vaccine and has already obtained positive outcomes of this therapy in mouse models of skin and lung cancers. Obviously, investigating the potential of this therapy against ovarian cancer holds great promise.
But first, how exactly does the dendritic cell vaccine work?
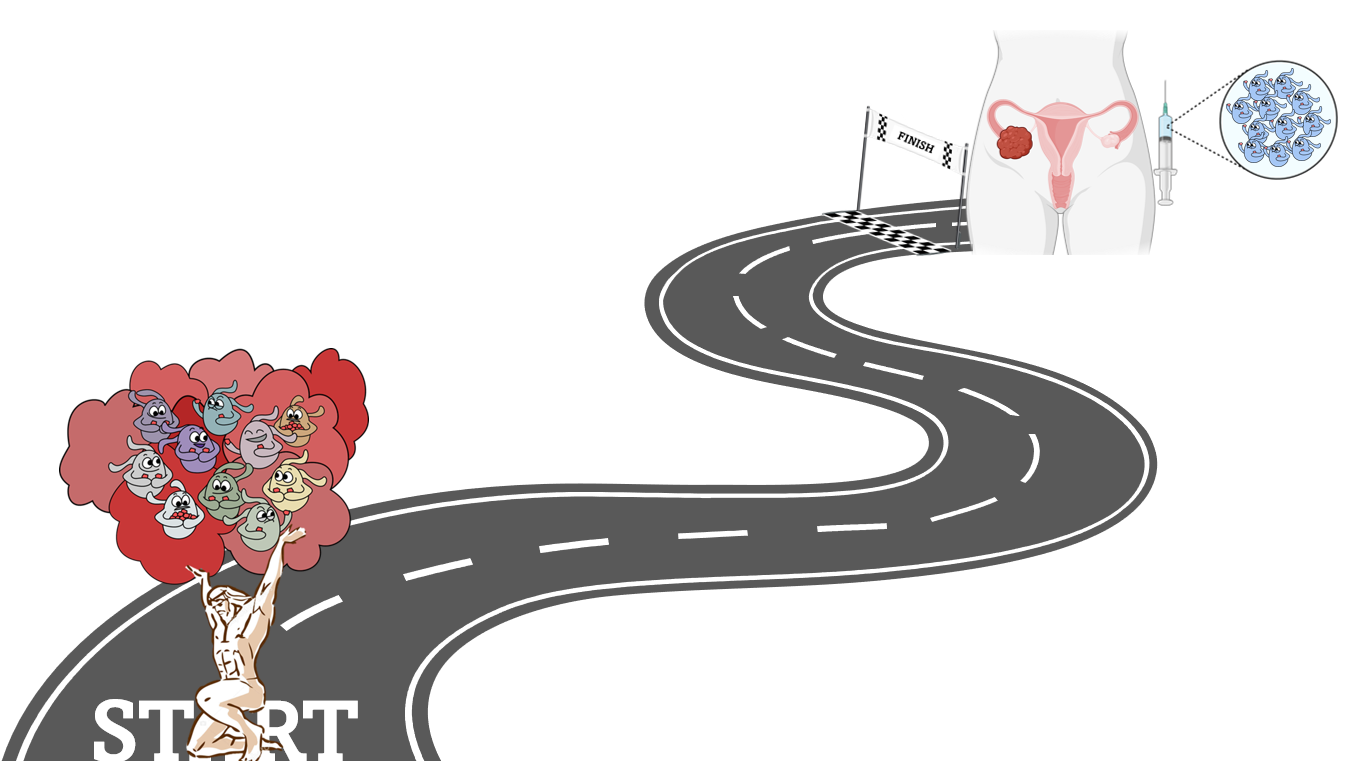
When a patient undergoes surgery to remove the tumor, we aim to specifically isolate the dendritic cells from the tumor and give them back to the patient as a vaccine. Since these dendritic cells have lived inside the tumor itself, they will have captured all the information needed to identify the cancer cells and when given as a vaccine they can transfer this information to the killer cells. The great thing is, these new anti-cancer killer cells can stay in the body for years. So, if some cancer cells return at some point in the future, these new killer cells can identify and destroy them.
But the obvious question remains: why did the dendritic cells not do their job in the first place? Why do they need to be taken out of the tumor only to be given back to the patient? Well, the cancer cells can prevent the immune cells from performing their regular functions. So, in the presence of the tumor, the dendritic cells fail to detect that the tumor is an issue. Or, if they detect it as an issue, they cannot report it to the killer cells. So by removing the dendritic cells from the tumor and giving them back to the patient in a cleaner tumor-free environment, they can function at their best.
Of course, it all sounds very promising. However, there is a small catch. The dendritic cells within tumors (of all cancer types) are not all identical. They come in several different types, each differing in abundance and function from the other. So, we broadened our horizons to include other cancers in addition to ovarian cancer and generated a tumor dendritic cell atlas, where instead of having a physical bound collection of geographical maps, we have a virtual collection of maps, only this time they are called UMAPs. Same same, but different!
How did we generate this atlas?

Very simply, we looked at all the genes present within all the tumor dendritic cells. By evaluating the similarities and differences between the genes from different cells we were able to distinguish and classify the different dendritic cell types. This technique is called single-cell RNA sequencing.
But what can we do with this atlas?
We can use the atlas for several applications but in terms of dendritic cell vaccinations, we can use it to study two main aspects, quantity and quality. For instance, if we intend to use a particular dendritic cell type as a vaccine, using the atlas we can get a first glance into whether or not they are present in sufficient numbers in a particular cancer. We can also gain insights into the quality of the dendritic cells by predicting their potential functions using in silico analysis of their genes. This way, the atlas can serve as a starting point to decide which might be the best dendritic cell type to be used as a vaccine against a particular cancer type.
With the tumor dendritic cell atlas at our disposal and existing research that tumor dendritic cell vaccines show benefits in mouse models of other cancers, what is the next step? Evidently, it is to test the dendritic cell vaccines in ovarian cancer. For this, we have generated a mouse model that largely resembles advanced-stage ovarian cancer patients, including the development of ascites (a bloody fluid that accumulates in the belly) and the spread of the cancer to the lungs. As mentioned, 80% of ovarian cancer patients are diagnosed at these advanced stages, hence it's this category of patients we aim to target with our therapy. In the near future, we want to test dendritic cell vaccination in our newly generated mouse model for ovarian cancer to assess its therapeutic potential.
All in all, we have generated a roadmap where our tumor dendritic cell atlas serves as the starting point toward better anti-cancer therapies against ovarian cancer. Using our ovarian cancer mouse model that is highly translatable to patients, we aim to test our dendritic cell vaccine in the hope that advanced-stage patients can live much longer than five more years.
Want to be kept up-to-date on our biotechnological news and stories? Join our community and subscribe to our bi-monthly newsletter.
Interested in becoming a part of the impactful work happening at VIB? Check out the available positions here..jpg)
Aarushi Audhut Caro