Not by the book
Cancer exploits the body's biological mechanisms – but differently.
By Ilse Boeren
This article originally appeared in Dutch in EOS Magazine. Read more at eoswetenschap.eu.
The era when researchers believed that cancer consists solely of cells multiplying wildly is definitively over. Scientists at the VIB – KU Leuven Center for Cancer Biology are studying inflammatory responses because cancer uses similar mechanisms but in a different way. This approach offers insights into new treatments, even for pancreatic cancer, notorious for its poor survival rate.
The coffee corner on the ninth floor of a new lab tower on the Gasthuisberg campus is the meeting point for researchers, sometimes joined by journalists. Kathryn Jacobs and Marcello Delfini plan to meet there to discuss their research. Do cancer researchers – because that’s what they are, each in their own domain – have a great need for caffeine?
‘Research is certainly a challenge because everything you discover is new.’ Delfini, a biotechnologist specializing in immunology with a deep affection for macrophages – 'the most beautiful cells of the immune system' – describes their work as putting together a puzzle without the box. ‘You know all the pieces must fit, but you have no example to guide you.’
American postdoc Jacobs, who focused on glioblastomas (brain tumors) during her PhD, now specializes in the biology of unique blood vessels in tumors and lymph nodes. She shares Delfini’s perspective. ‘I discovered during my PhD that what you learned in school can be forgotten when working with tumors, especially regarding signal pathways. Tumors don’t follow the book.’
Initially, cancer research revolved around how a cell could begin dividing wildly. Therapies merely halted and killed cancer cells. ‘Chemotherapy and radiotherapy create genetic instability, increasing mutations in rapidly dividing cells,’ explains Delfini. ‘These therapies, affecting all rapidly dividing cells – hair, skin, eyes – result in significant side effects.’
Hijacked immune system
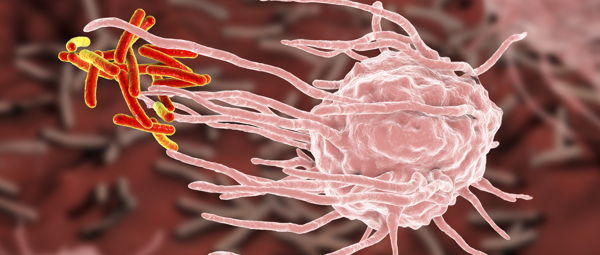
Although it’s true, of course: cancer cells proliferate in an uncontrolled manner, and they do not die. 'For embryonic development, but also for the stable state of organs, cell death is crucial, and cancer cells manage to avoid it.' In the 1980s, it became clear that tumors hijack our body's immune response to preserve everything positive for tumor growth and cancer cell metastasis while blocking everything negative for it.
However, it is essential to note that a tumor doesn't primarily consist of rapidly dividing cancer cells. Thinking so is naive, according to the researcher. ‘Now we understand that a tumor is a complex system, it has blood vessels to supply nutrients and fibroblasts for structure and strength. There are many stromal cells, differentiating cells promoting tumor growth, and an incredible number of immune cells inside the tumor, primarily macrophages – their share can go up to sixty percent.’
The discovery that immune cells infiltrate cancer tissue and that the immune system can recognize and kill cancer cells led to the introduction of immunotherapy. A game-changer, according to Delfini, ‘but unfortunately, it only works for some patients. Many people are resistant to immunotherapy.’ Additionally, some cancers are challenging to treat. The life expectancy of pancreatic cancer, for example, is very short.
‘In our lab, we are researching mechanisms of resistance to immunotherapy through the tumor microenvironment,’ continues the researcher. ‘The various cell types in a tumor are not scattered independently; they form an ecosystem, a complex network of interaction. And the metabolic pathways they develop significantly impact how well immunotherapy works.’
Cancer, on the one hand, suppresses the immune system's anti-tumor response by hijacking mechanisms that temper the immune response to avoid autoimmune diseases. On the other hand, it takes over the wound-healing process, another function of the immune system. ‘Maintaining or returning to homeostasis, the normal state, so to speak. When this was discovered, researchers likened cancer to a wound that never heals.’

In its favor
This is where the connection with inflammatory responses lies. It's a very broad term. The scientific definition of inflammation is the body's response when homeostasis is disrupted for any reason, aiming to return it to its original state. First, the immune system must assess the situation. Is there an infection, are there pathogens that need to be cleared? Afterward, when all pathogens are gone, the wound should close.
‘All these things also happen in cancer,’ explains Delfini. ‘It needs an anti-inflammatory environment because cytotoxic T-cells should not be activated to destroy the cancer cells. It exploits the wound-healing response. The tumor needs to grow, requires blood vessels and structure. Cancer can utilize processes encoded in our biology for repair to its advantage.’
‘That's what the cancer cell understands.’ Delfini quickly clarifies his statement: a cancer cell, of course, understands nothing; it's just a cell. ‘But evolutionarily, cancer cells that can exploit such a mechanism to their advantage will multiply more than others. Thus, cancer learns during its evolution.’
Kathryn Jacobs also witnessed an example of the extreme adaptability of cancer cells during her doctorate. ‘Cancer stem cells exist. During chemotherapy and radiation, these cells no longer divide; they simply wait until the therapy is over. Then they reproduce, but their descendants are adapted to the chemotherapy and radiation, and they don't die anymore.’
The various cells in a tumor share the common goal of trying to survive in a hostile environment. A significant advantage in this endeavor is the enormous mutation rate of cancer. ‘It can, for instance, switch from glucose metabolism to fatty acid metabolism or vice versa.’ According to Jacobs, that's why many research groups focus on ways to strengthen our immune system instead of targeting the cancer cells themselves. ‘They change too quickly. Our research group also aims to stimulate the immune system,’ she continues. ‘We want to make the blood vessels in tumors immune-stimulating so that immune cells can enter. In our ideal scenario, we induce high endothelial venules (HEV) and get even more immune cells.’
An extra lymph node?
Jacobs' research focuses on the biology of these high endothelial venules. Venules are microscopic blood vessels that collect oxygen-poor blood from the capillaries and send it to the veins. High endothelial venules are a special type of venule with an inner layer (endothelium) of cuboid-shaped cells. During infection, they provide more lymphocytes, T-immune cells, and B-immune cells in the lymph node. All these cells pick up the antigen signal, increasing the efficiency of the fight against everything they need to combat in the body.
‘Several years ago, it was discovered that these blood vessels occur not only in lymph nodes and secondary lymphoid organs but also in extraordinary places in the body. They form during inflammatory reactions. You can get them, for example, in your lungs or if you have a rash on your skin. They also have their familiar function there: they bring many immune cells to that location.’ In inflammations, this could worsen the prognosis as patients receive too many immune cells. But if HEV develops in the tumor, it actually improves the prognosis.
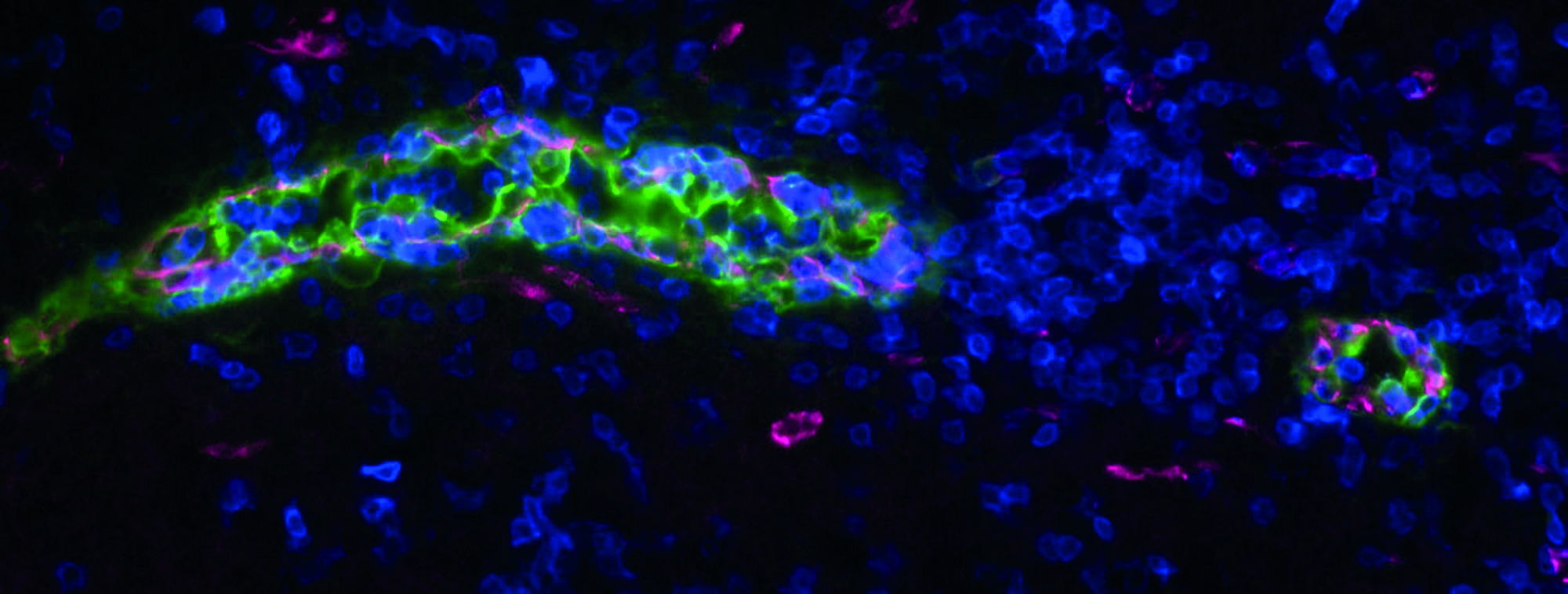
‘Cancer drives away the immune system. Extra HEV can counteract immune suppression by bringing in more T-cells and B-cells. Normally, blood vessels in a tumor have unique surface markers encouraging immune cells to pass through the tumor. If immune cells do come out in the tumor, that's great; they can attack the tumor. Last year, our lab published an article on treatments to induce the formation of HEV in the tumor.’
Previously, researchers believed that anti-angiogenic therapy, reducing blood vessel formation, would kill the tumor. ‘They thought the tumor would starve.’ However, they discovered that blood vessels in the tumor became healthier, allowing immune cells to enter more effectively. ‘We also used anti-angiogenic therapy and added an immune checkpoint blockade. The latter blocks the signal telling immune cells not to do their job.’ The research yielded positive results for breast cancer, melanoma, and colorectal cancer, all in mouse models.

In its favor
Jacobs focuses her research on how HEV forms in the tumor and in lymph nodes. ‘The lymph node has places where B immune cells and T immune cells are concentrated around the HEV.’ The research group observed the same in a tumor: B-cells, T-cells, and HEV together in an organized structure. ‘We call this a tertiary lymphoid structure, TLS. Tumors with these structures have the best prognosis for recovery. So now we are looking for a therapy to induce TLS.’
‘Simultaneously, in our lab, we examine HEV and their functional biology in the lymph node and how it relates to that in the tumor.’ A notable observation is that HEV in the tumor closely resemble inflamed HEV in the lymph node. ‘In retrospect, that makes sense because the tumor is an inflammatory environment.’
Less lactic acid
Delfini's team has also made strides toward new therapies, approaching the challenge from the perspective of inflammatory biology. One of the PhD students in the group, Federica Cappellesso, found a way to loosen the brakes on the immune system in mice with pancreatic cancer. ‘Because the immune system is potent in destroying anything not belonging in the body, it must be tightly regulated. Our body cannot risk becoming active against something that shouldn't be destroyed – which is the case in autoimmune diseases.’
T-immune cells have a self-regulating mechanism preventing excessive damage. If they repeatedly kill the same antigen, they become exhausted and stop attacking. ‘The problem is that there are many tumor cells in a tumor. T-cells, therefore, exhaust quickly. We wondered how we could counteract the exhaustion of T-immune cells. Think of it as the cup of coffee we drink when tired but facing a deadline.’
The primary immunotherapy today involves anti-PD-1 antibodies. ‘The PD-1 receptor is an immune checkpoint; it provides a negative signal for T-lymphocytes. If PD-1 is active in the T-cell, it becomes exhausted. The study I find fascinating focused on pancreatic cancer. However, it doesn't work well. The reason is that not many T-cells penetrate the pancreatic cancer tissue. If there are no T-cells in the cancer tissue, you can keep telling them, 'Don't get tired.' It won't help.’
Cappellesso discovered that pancreatic cancer has a challenging microenvironment. ‘Pancreatic cancer cells have a specific transport protein they use to import bicarbonate.’ Bicarbonate is a potent pH buffer. ‘This allows cancer cells to maintain a neutral pH in their interior. They can perform more glycolysis, produce more energy, and multiply more.’ Simultaneously, they produce more lactic acid, the waste product of their metabolism.
‘Not only can they produce more lactic acid, but they can also export more lactic acid. The drop in pH outside the cell, due to the presence of a lot of lactic acid and little bicarbonate, creates an acidic microenvironment where T-cells cannot function.’ The researchers succeeded in blocking the transport protein, doing something detrimental to cancer cells. ‘They have fewer opportunities to maintain their pH neutral, reducing their metabolic capacity. But T-cells benefit as well. Less metabolism means less lactic acid emission. Along with the reduced bicarbonate import, it creates a less acidic environment outside the cell, allowing T-cells to function normally there.’
(No) way out
The significant advantage of such therapies – besides their efficacy against challenging cancers and providing an escape from immunotherapy resistance – is their minimal side effects. ‘That transport protein, our target, is highly specific to pancreatic cancer. We can slow down its function without causing significant changes in the patient's overall body.’
And for the patient, the researchers press on. ‘We are in the process of patent applications because the outcome of our research must reach the public; it must reach the people.’ Delfini sees this as the significant advantage of working for VIB. ‘Understanding the processes is beautiful in itself, but the fact that our science finds an application is crucial to me.’
It will still take some time. ‘You know how it goes. First, years of work by our PhD students, then fine-tuning and patent applications. After that, a pharmaceutical company can take it up to create a drug. But it still needs to go through clinical trials.’ Delfini finds the result worth all the time, money, and effort, even though he originally never intended to become a cancer researcher. ‘I wanted to do something completely different. But this research is so beautiful. Suddenly, I was in the middle of it, and there was no way out.’
Want to be kept up-to-date on our biotechnological news and stories? Join our community and subscribe to our bi-monthly newsletter.
Read more