"The next step was to see if changing the intestinal bacteria composition could have a positive effect on Parkinson's disease"
On Parkinson's disease, the gut microbiome, and fecal microbiota transplants
Today, April 11, is World Parkinson's Disease Day. The day, organized by the International Parkinson and Movement Disorder Society aims to raise awareness and understanding about Parkinson's disease (PD).
- Parkinson's disease is a neurodegenerative disorder in which the brain slowly loses the ability to produce dopamine, which causes a variety of motor symptoms, like tremors, rigidity, and slow movements.
- Worldwide, roughly 10 million people have the condition, and it affects up to 2–3% of people over 65. Still, one in ten Parkinson's patients is under 50 years old.
- It is the fastest-growing neurological condition in the world.
- Current treatments only manage symptoms, mainly through dopamine replacement.
- Growing evidence links gut microbiome alterations to PD, as gastrointestinal dysfunction often precedes motor symptoms.
The link between the gut microbiome and PD symptoms and disease progress is a research topic for VIB researchers. Last year, the team of Roosmarijn Vandenbroucke (VIB-UGent Center for Inflammation Research), together with neurologists Patrick Santens and Arnout Bruggeman (UZGent), reported on the potential of fecal microbiota transplants for improving symptoms in PD patients.
Based on this and other work, she teamed up with Jeroen Raes (VIB-KU Leuven Center for Microbiology) and colleagues from UGent, KU Leuven, UZ Gent, UZ Leuven, and the Leiden University Medical Center. Supported by VIB's Grand Challenges program, their CUPIDGUT project will further explore the use of fecal microbiota transplants in the treatment of Parkinson's disease. In a multicenter study, the researchers will refine the procedure, identify biomarkers that can signal treatment success, and develop clinical guidelines for widespread adoption.

For some background on the Parkinson-gut connection and the CUPIDGUT project, we asked Arnout Bruggeman a few questions. Arnout is a neurologist at VIB-UGent-UZGent who participates in CUPIDGUT.
Where did the idea to use fecal microbiota transplants in the treatment of Parkinson's disease come from? Which observation was the initial spark?
Arnout: "Parkinson's disease is mainly known for its motor symptoms caused by problems in the brain. But the vast majority of patients frequently experience problems in the gastrointestinal tract as well (already noted in the first description of the disease by James Parkinson). These gastrointestinal symptoms often develop years before there are movement problems, and seem to be an early symptom of the disease. That is why people have started to look more and more at the intestines, to find out whether the gastrointestinal tract has anything to do with the development of the disease.
And since 2015 we know that the intestinal bacteria composition of patients has clearly changed compared to people without Parkinson's disease. The next step was to see if changing the intestinal bacteria composition could have a positive effect on the course of the disease. This was of course first tested in laboratory animals, and given the positive results this then led to clinical studies in humans."
What does a fecal microbiota transplant look like in practice?
Arnout: "A long, thin tube is inserted through the nose (with a lot of gel), which is then guided via the esophagus and stomach into the small intestine. The procedure itself is 'more pleasant' than a classic stomach examination - the tube in a stomach examination is thicker and must be inserted through the mouth, which is less well tolerated (we bypass the gag reflex by entering through the nose). As soon as the tube is in the right place, the fluid is injected very slowly so that people do not actually feel it. The transplant solution is in a large syringe that is connected to the tube. That syringe is covered, so people do not see the color. The process is also odorless and does not require anesthesia. The people lie half-sitting on their backs on an examination table. After everything has been injected, the people remain lying down for a while, then the tube is removed, and they can go home."

Why would it work? What is the (hypothetical) link between the gut microbiome and Parkinson's disease?
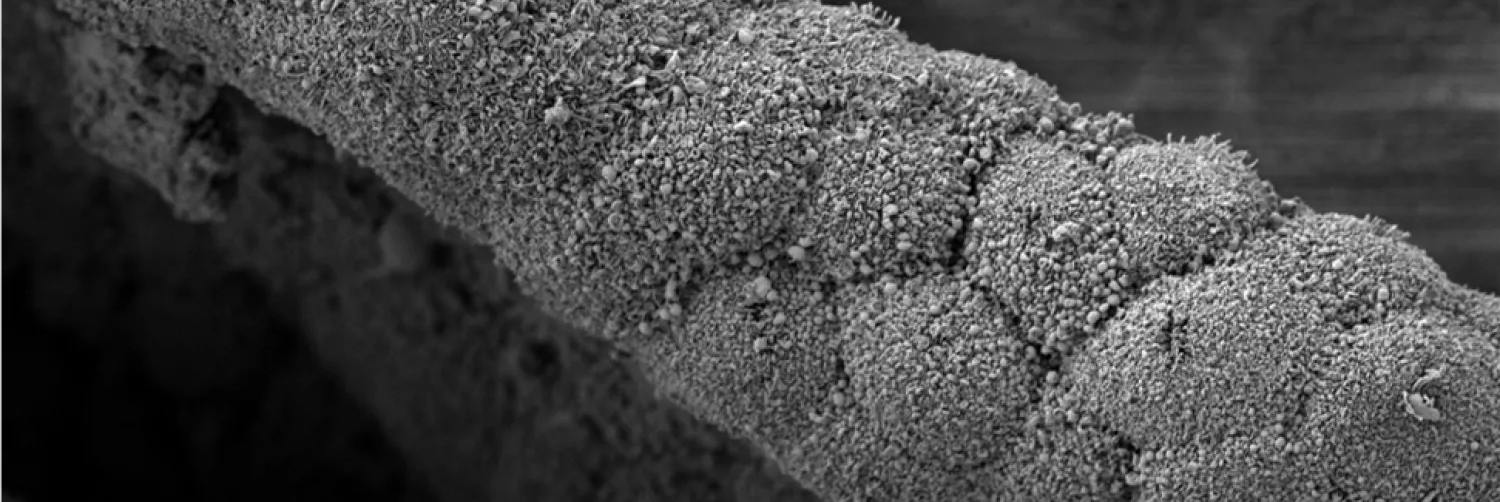
Arnout: "In the intestines themselves, we can see signs of intestinal inflammation, a reduced integrity of the intestinal wall barrier, and the accumulation of the protein α-synuclein. This protein also accumulates in the brain and is considered characteristic of the disease. It has already been shown that these α-synuclein deposits in a group of patients were clearly present first in the intestines, and only later in the brain.
All these connections between the intestines and Parkinson's disease have led to research into the intestinal bacteria. The idea is that by restoring the gut microbiota composition, we can impact these negative changes in the gut and their subsequent effects on the brain."
If we assume everything goes well and you find a crucial link between the composition of the gut microbiome and Parkinson's disease progression, how would that ideally impact patients' lives?
Arnout: "At the moment, there are only symptomatic treatments for Parkinson's disease. So there are no treatments yet that can slow down or stop the disease process. Research is being done in various areas, but we hope that the findings from the gut microbiome can lead to such disease-modifying treatments.
The impact on quality of life increases as the disease progresses. So, a disease-modifying treatment will have a major impact on quality of life. Of course, additional symptomatic treatments are always welcome, but symptomatic treatments are not the ultimate goal."
Finally, if there is one misunderstanding about Parkinson's disease you wish people would stop believing, what would it be?
Arnout: "Parkinson's disease is still seen too much as 'a disease of old people' while it also affects a lot of relatively young people. The average age of diagnosis is around 60 years, so it also affects a lot of people who are still young and working. It is also the fastest growing neurodegenerative disease, so the problem is also getting bigger... Time to do something about it..."
Find out more about the CUPIDGUT project.
Gunnar De Winter